Solution Overview
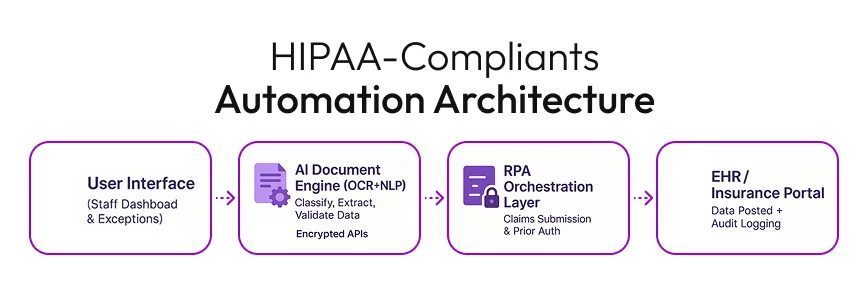
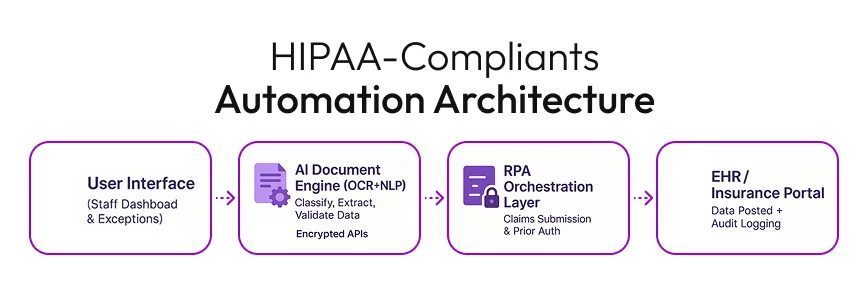
To transform the administrative backbone of this healthcare network, we deployed a HIPAA-compliant AI document automation ecosystem.
Key Features Implemented:
- AI Document Processing:
Leveraged OCR and AI-powered classification to digitize and interpret unstructured documents. - No-Code Automation Platform:
Used low/no-code tools to orchestrate workflows, cutting development time and costs. - Secure EHR Integration:
Direct push of validated data into the provider’s EHR (Medgen/Epic/Cerner) using secure APIs. - Robotic Process Automation (RPA):
Configured bots to automatically handle claims submissions, eligibility verification, and prior authorizations. - Exception Handling:
Established human-in-the-loop review queues for flagged documents or mismatched data. - Audit and Compliance Layer:
Built-in logging, encryption at rest/in transit, and access controls meeting HIPAA/HITRUST standards.
Detailed Workflow
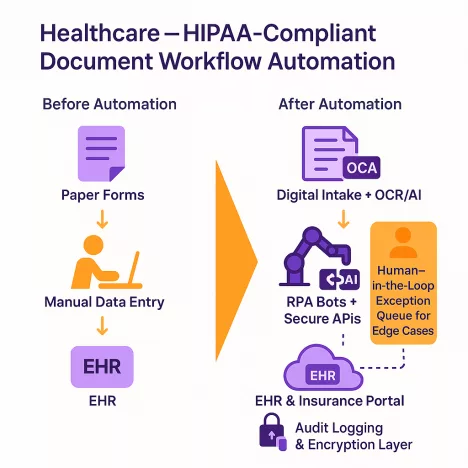
| Step | Before Automation | After Automation |
|---|---|---|
| Patient Intake | Manual scanning and data entry | AI reads & validates, pushes to EHR |
| Claims Submission | Staff uploads to multiple portals | RPA bots auto-submit with tracking |
| Prior Authorization | Fax & phone calls to insurers | Automated request submission with status updates |
| Compliance Audit | Manual log collection | Real-time audit-ready dashboards |
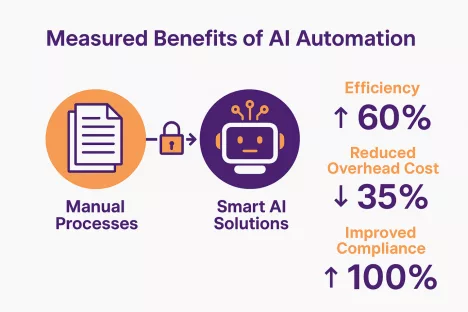
Impact and Measured Benefits
- Reduced Processing Time by 60%– Patient data now reaches clinicians faster, improving care coordination.
- Cut Administrative Overhead by 35%– Freed up staff for higher-value patient interaction.
- Improved Compliance Readiness to 100%– All workflows now have encryption, access controls, and full audit trails.
- Increased Data Accuracy– Error rate in claims dropped dramatically due to AI validation.
- Scalability & Flexibility – New document types or insurer portals can be added in days instead of months.
Key Takeaways for Similar Organizations
- Start Small, Scale Fast:Begin with one high-volume document type, prove the ROI, then expand.
- Design for Compliance:Embed HIPAA/HITRUST requirements early—don’t retrofit later.
- Human + AI Synergy:Automation should complement staff, not replace them.
- Visibility Matters:Dashboards and audit trails make compliance and performance tracking painless.
Solution Overview
Solution Overview
To transform the administrative backbone of this healthcare network, we deployed a HIPAA-compliant AI document automation ecosystem.
Key Features Implemented:
- AI Document Processing:
Leveraged OCR and AI-powered classification to digitize and interpret unstructured documents. - No-Code Automation Platform:
Used low/no-code tools to orchestrate workflows, cutting development time and costs. - Secure EHR Integration:
Direct push of validated data into the provider’s EHR (Medgen/Epic/Cerner) using secure APIs. - Robotic Process Automation (RPA):
Configured bots to automatically handle claims submissions, eligibility verification, and prior authorizations. - Exception Handling:
Established human-in-the-loop review queues for flagged documents or mismatched data. - Audit and Compliance Layer:
Built-in logging, encryption at rest/in transit, and access controls meeting HIPAA/HITRUST standards.
Detailed Workflow
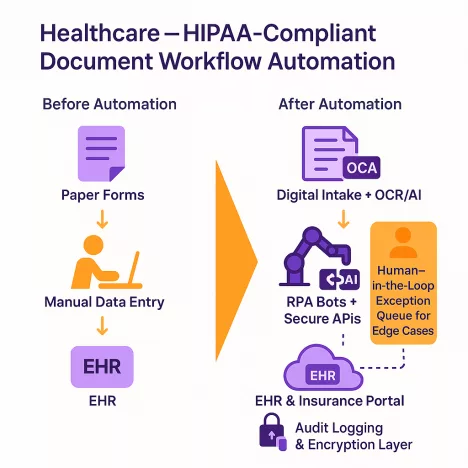
Detailed Workflow
| Step | Before Automation | After Automation |
|---|---|---|
| Step | Before Automation | After Automation |
| Patient Intake | Manual scanning and data entry | AI reads & validates, pushes to EHR |
| Claims Submission | Staff uploads to multiple portals | RPA bots auto-submit with tracking |
| Prior Authorization | Fax & phone calls to insurers | Automated request submission with status updates |
| Compliance Audit | Manual log collection | Real-time audit-ready dashboards |
Impact and Measured Benefits
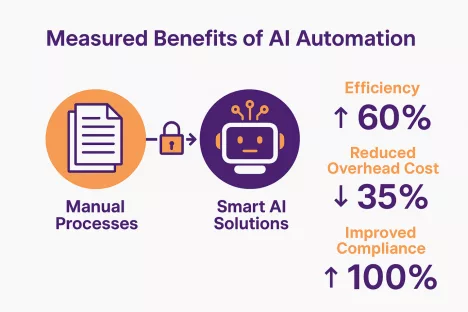
Impact and Measured Benefits
- Reduced Processing Time by 60%– Patient data now reaches clinicians faster, improving care coordination.
- Cut Administrative Overhead by 35%– Freed up staff for higher-value patient interaction.
- Improved Compliance Readiness to 100%– All workflows now have encryption, access controls, and full audit trails.
- Increased Data Accuracy– Error rate in claims dropped dramatically due to AI validation.
- Scalability & Flexibility – New document types or insurer portals can be added in days instead of months.
Key Takeaways for Similar Organizations
Key Takeaways for Similar Organizations
- Start Small, Scale Fast:Begin with one high-volume document type, prove the ROI, then expand.
- Design for Compliance:Embed HIPAA/HITRUST requirements early—don’t retrofit later.
- Human + AI Synergy:Automation should complement staff, not replace them.
- Visibility Matters:Dashboards and audit trails make compliance and performance tracking painless.